Aesthetic consultations are increasingly focused on safety, precision, and individual anatomy. As facial assessment becomes more sophisticated, ultrasound technology has emerged as a valuable tool to support deeper anatomical understanding in selected cases.
While ultrasound is not required for every consultation, its use reflects a commitment to evidence-based, anatomy-led aesthetic care.
Understanding the Complexity of Facial Anatomy
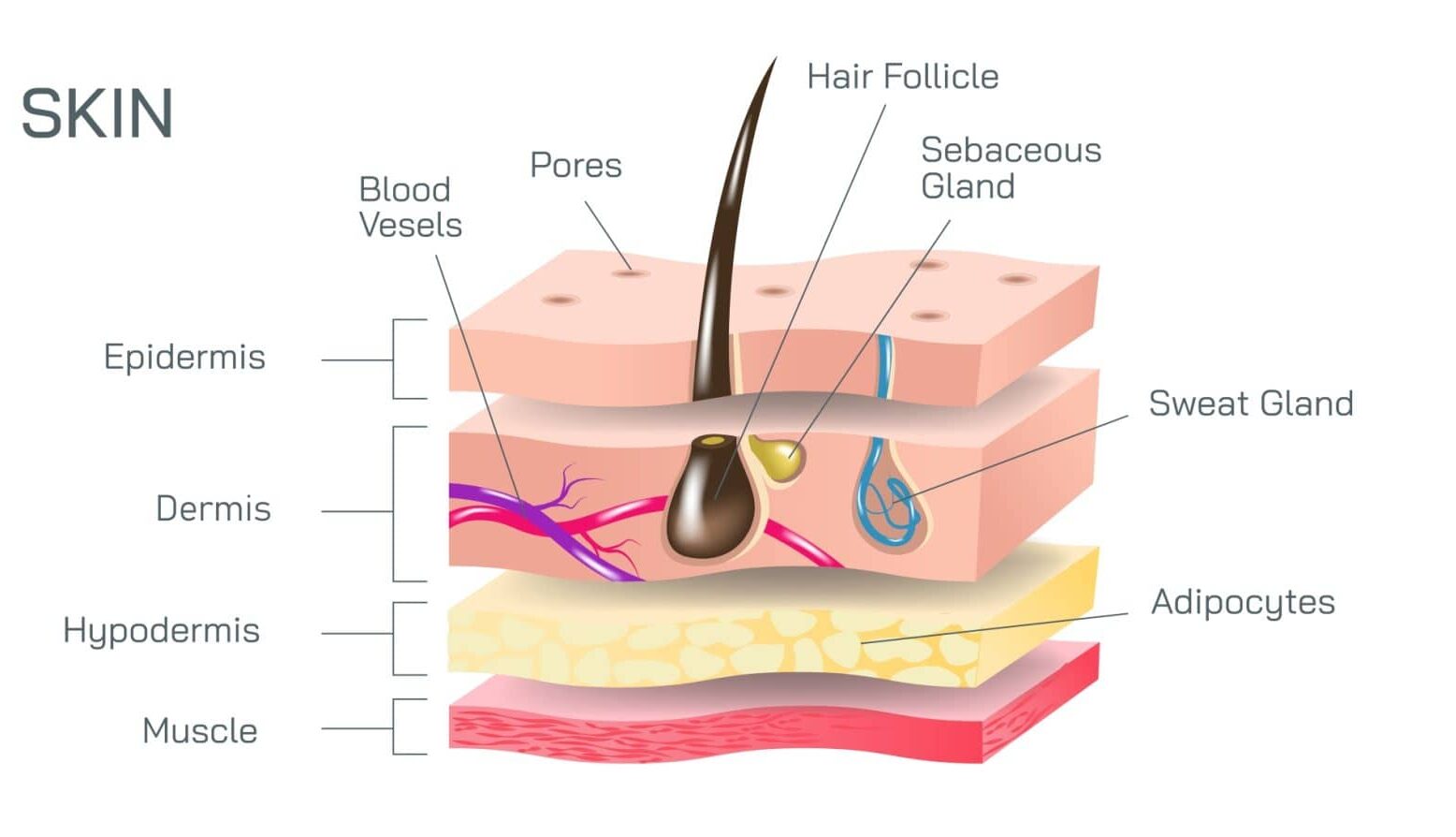
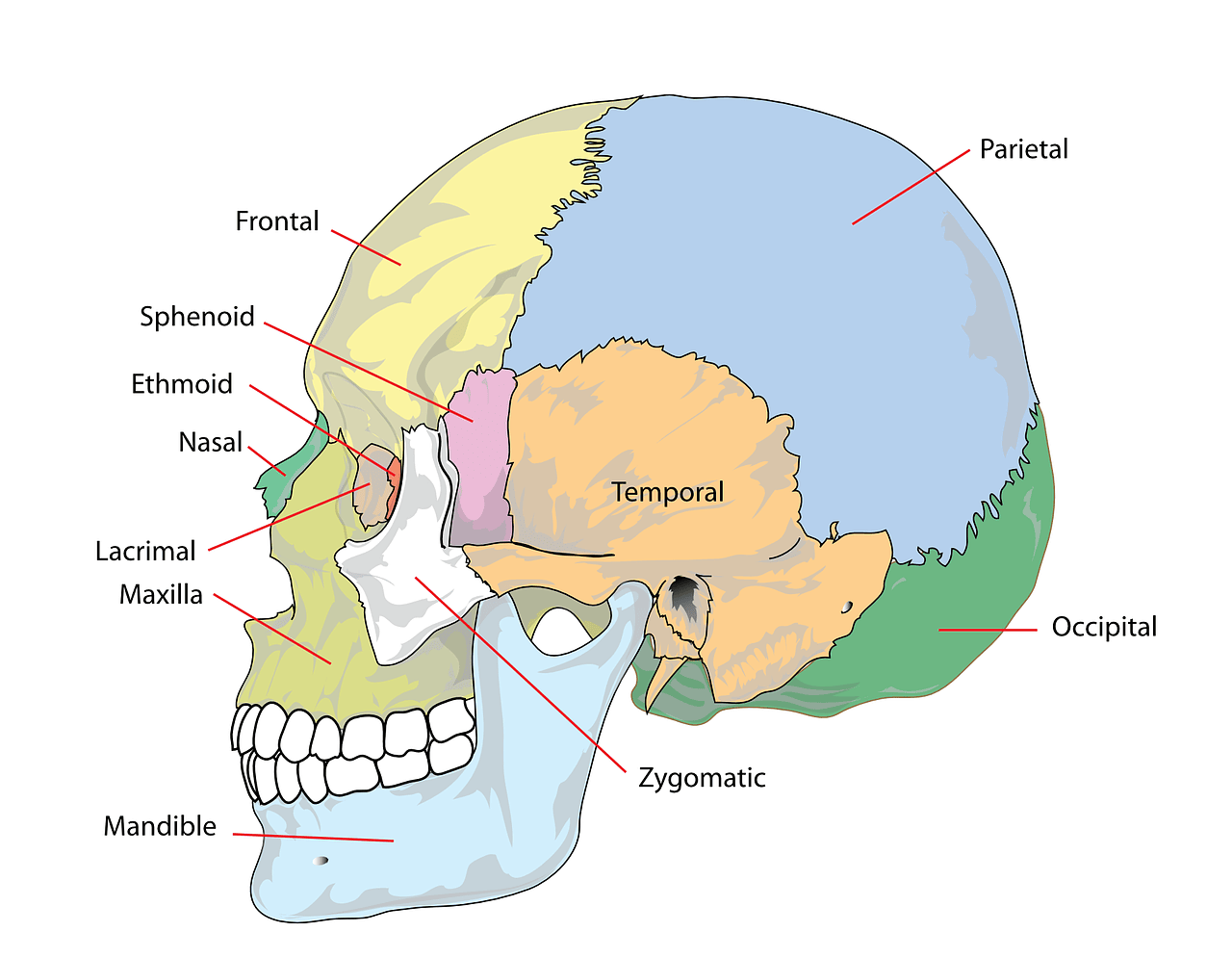
The face contains a complex network of muscles, blood vessels, fat pads, and connective tissue layers. These structures vary significantly between individuals and change over time due to ageing, previous treatments, and natural anatomical differences.
Visual assessment alone does not always provide complete information about what lies beneath the skin. Ultrasound allows clinicians to visualise underlying structures in real time, supporting a more informed assessment.
What Is Aesthetic Ultrasound?
Aesthetic ultrasound is a non-invasive imaging technique used to view soft tissue structures beneath the skin. It can help identify:
- Blood vessels and their depth
- Fat compartments
- Muscle
- Bone
- Foreign body implants, where relevant
This information supports safer planning and more personalised consultation discussions.
When Ultrasound May Be Used During a Consultation
Ultrasound is not necessary for every patient or every concern. It may be considered when:
- There is complex facial anatomy
- Previous treatments have been performed
- Additional anatomical clarity is beneficial
- Safety considerations require further assessment
The decision to use ultrasound is made on an individual basis as part of a comprehensive consultation.
Ultrasound and Patient Safety
Safety is central to aesthetic care. By improving anatomical understanding, ultrasound can support:
- More informed treatment planning
- Identification of high-risk areas
- Increased confidence in anatomical decision-making
Its use reflects a careful, assessment-led approach rather than a standardised or routine protocol.
Why Ultrasound Supports Consultation-Led Care
Current regulatory frameworks emphasise that decisions involving prescription-only medications must be made by a qualified health professional in consultation with the patient.
Ultrasound aligns with this model by:
- Supporting personalised assessment
- Reinforcing treatment decisions on individual anatomy
- Reducing reliance on assumptions or trends
This approach prioritises education, suitability, and individualised care.
Final Thoughts
Ultrasound is not about offering more treatment — it is about understanding anatomy more clearly. When used appropriately, it supports more informed aesthetic consultations and reflects a commitment to evidence-based practice.
If you’re considering a consultation for volume loss consultation, ultrasound technology can support a personalised anatomy assessment, discussing suitability, treatment options, and individual considerations.
Frequently Asked Questions
No. Ultrasound is used selectively when additional anatomical information is helpful. Its use depends on individual anatomy, history, and clinical considerations.
No. Ultrasound complements, rather than replaces, clinical assessment. Visual examination, palpation, and discussion remain essential components of a consultation.
Ultrasound is a non-invasive imaging tool commonly used in medical settings. When used appropriately, it is considered safe and well tolerated.
Ultrasound requires specialised training, experience, and equipment. Its use reflects a practitioner’s commitment to anatomy-led and safety-focused care.
Ultrasound supports informed decision-making by improving anatomical understanding. This can enhance safety and planning, but outcomes always depend on individual factors and suitability.